Obamacare will add 7 million insured in CA
March 14, 2013
By Katy Grimes
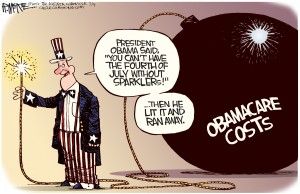
SACRAMENTO — With Obamacare implementation looming, and California’s open-arms embrace of what’s officially called the Affordable Care Act, as many as 7 million new people will access healthcare in the state by 2014. The new patients will worsen the existing shortage of primary care physicians, and will undoubtedly drive up health care costs even more.
California legislators are looking at one possible solution: Expanding the “scope of practice” for California’s para-professional medical practitioners — nurses, licensed vocational nurses, nurse practitioners, and physician assistants — along with optometrists and pharmacists.
This solution is not new and also came up in hearings last year.
California’s Obamacare legislation
State Sen. Ed Hernandez, D-West Covina, an optometrist and chair of the Senate Health Committee, introduced three “scope and practice” bills Wednesday to address the doctor shortage. But it was quickly evident there will be a battle with physicians over this “scope of care,” and what the role of professionals versus para-professionals will be in the future.
“Here in the state of California, we have a capacity issue. We have a work-force shortage,” Hernandez said at the hearing. He warned the problem is already at a breaking point in inner-cities, as well as rural parts of the state. Up to 7 million uninsured Californians will be required to be insured as of next year.
“How is it that we’re going to be requiring somebody to purchase health insurance, but yet they won’t have access to a doctor?” Hernandez asked at the hearing. “This is what we need to address.”
“We are working hard at the state level to ensure every Californian has access to affordable, quality health coverage, but what good is a health insurance card if you can’t get into see a health care provider when you need one?” said Hernandez, “We need to make better use of the trained healthcare workforce we already have if we are ever going to meet demand.”
Joint Senate hearing
Wednesday’s joint committee hearing was held with the Senate Health Committee and Business and the Professions and Economic Development Committee. The joint committee heard from a medical doctor representing the California Medical Association, an attorney for the University of California, San Francisco’s Center for the Health Professions, a physician assistant, a pharmacist and an optometrist. Each speaker was compelling and supported expanding the scope of practice in order to accommodate the massive increase in patient access.
Hernandez said he invited representatives from these areas of practice to speak because “they have rigorous training standards, are evenly distributed across the state, have a proven record of providing quality care, and are regulated by independent boards that will make certain patient safety is not compromised.”
Catherine Dower with UCSF warned that the implementation of Obamacare in California will put additional strain on the primary care physician workforce, particularly in the poorer inner-city areas and rural locations. Dower referred to a study by the Institute of Medicine which found the barriers should be removed from the nursing “scope of practice,” allowing more nurses to expand responsibilities.
Dower said a diverse mix of healthcare providers will be needed, and referenced former U.S. Sen. Tom Daschele’s blog post last week. Daschele, now a lobbyist, recommended expanding the “scope of practice” for all primary care providers, including nurses.
Daschele also recommended giving the government more power over decision making. “As a better understanding of the appropriate mix of additional providers is acquired, the National Health Care Workforce Commission that is called for in the Affordable Care Act should make specific recommendations to the Secretary of Health and Human Services,” he said. The Secretary should then be empowered, subject to Congressional review and legislative veto, to raise or lower the ceiling based upon an annual assessment of workforce availability and the long-term projected demand for health care services.”
Physician recommendations
The highlight of the hearing was Jeremy Fish, M.D. Fish, the residency director for the Contra Costa Family Medicine Residency, had some realistic recommendations for dealing with the primary care physician shortage, including expanding some nursing responsibilities. Fish explained the importance of a team approach to family practice medicine, which includes doctors, licensed vocational nurses, nurse practitioners, physician assistants, mental health providers and pharmacists. And Fish said the need for more medical residency programs in counties throughout the state was crucial.
Fish explained that most doctors either set up practice where they grew up or near where they went to school. “We practice close to where we trained,” Fish said. “Fragmentation is causing problems even within physician groups.”
He explained it would be relatively easy and less expensive in the long run to set up medical residencies in outlying areas, as well as urban areas which do not have teaching hospitals. This would not only help physicians get the medical training they need, it would serve an already underserved area.
Additionally, he said, using the Kaiser Permanente model, more medical practices need to be in one building, not spread out all over a city or county. “If we lock ourselves in the same space, we get along much better,” Fish said. “The Mayo Clinic found that putting mental care providers in the same office as primary care practices improved the quality of care for the patient.”
State Sen. Cathlene Galgiani, D-Livingston, told about a program U.C. Merced is using in conjunction with U.C. Davis Medical School to get trained doctors to do residencies in the Merced area. The UC Merced San Joaquin Valley Program in Medical Education allows students to complete their first two years of medical school at U.C. Davis, then do the last two years in the rural parts of Merced County, while attending classes at U.C. Merced. Galgiani said it is a much lower cost program, and fills the gap of medical providers in the area.
High medical costs, lower reimbursements
While there is clearly much need for more primary care physicians in California, doctors expressed concern that lawmakers’ embrace of Obamacare will create even more problems, including higher costs. The cost of medical school is extreme. Students graduating with massive debt often look to medical practices which are more lucrative in order to pay off the debt.
Dr. Ruth Haskins addressed the low reimbursement rate of primary care physicians’ Medicare and Medicaid costs. She said the state needs to work more to keep such physicians living and working in California. “Medi-Cal reimbursements are so low in California, and we are facing a drop,” she said.
“This isn’t a hearing on economics,” retorted Sen. Bill Monning, D-Carmel, “but they are linked.”
Hernandez has introduced Senate Bills 491, 492 and 493, and Sen. Fran Pavley will be introducing Senate Bill 352, which would expand the “scope of practice” for physician’s assistants.
Another bill that’s returning is by Sen. Christine Kehoe, D-San Diego, to allow nurse practitioners, physicians assistants and certified nurse midwives to perform abortions.
Related Articles
N.Y. Times shames Mercury-News on AB 32 coverage
April 23, 2013 By Chris Reed The fact that no one in the California media besides me has reported that
Greenlining series: Another ACORN-like menace?
This is the fourth part of a series produced by CalWatchdog and the Examiner regarding the Berkeley-based Greenlining Institute, a